Polycythemia Vera (PV) is a chronic myeloproliferative neoplasm characterized by erythrocytosis, constitutively active mutations in JAK2 and an increased susceptibility to thrombotic events (TEs). There is still controversy about the role of increased hematocrit and of other variables including elevated white blood cell count as risk factors for the occurrence of TEs. A better definition of the relative prognostic importance of hematologic parameters would help us to better tailor the therapeutic approach to PV patients (pts), which is currently mainly based on the use of acetilsalycilic acid (ASA), venesection and hydroxyurea .
The aim of our study was to analyze if any clinical or laboratory variables were significantly associated to the occurrence of TEs both at PV diagnosis and during the course of the disease in a large series of PV pts uniformly followed at a single Center over a period of 29.5 years from January 1986 to June 2019.
Clinical and laboratory data were obtained from the time of diagnosis until death, progression to acute leukemia or last follow-up. Hematocrit (Hct), hemoglobin (Hb), white blood cell (WBC) and platelet (PLT) levels were recorded for each patient at least every 6 months.
Among a total of 331 pts, the median age was 65 years (range 30-92 years), and 56% were male. "High risk" features (age ≥ 60 years and/or history of prior thrombosis) were present in 221 pts (66.7%). The incidence of cardiovascular risk factors was: hypertension 64%, diabetes 15%, hyperlipidemia 28%, history of active or remote smoking 41%. Patients on ASA were 279 (84%), 19 (6%) were on oral anticoagulation, while 27 (8%) were on ASA+oral anticoagulant. At PV diagnosis 54 pts (16%) presented with thrombosis, arterial in 32 (59%) and venous in 22 (41%). A previous TE was recorded in 57 pts (17%): in 43 (75%) arterial, in 12 (22%) venous and in 2 (3%) mixed (arterial+venous). Previous thrombosis was the only variable significantly associated with the presence of a TE at PV diagnosis (P=0.02).
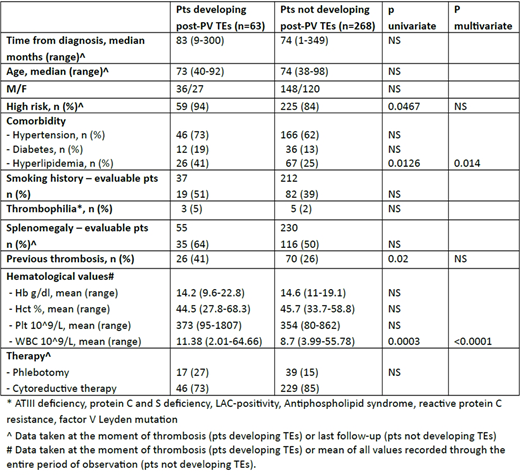
After PV diagnosis, with a median follow-up of 81 months (range 1-374 months), 63 pts (19%) experienced a TE and 11 of them a further episode, for a total of 74 TEs. The incidence rate (pts/year) of TEs was 2.7%. Forty-two events were arterial (57%), 31 were venous (42%) and 1 (1%) was mixed. It was the first TE for 37 pts. Cerebrovascular accidents and deep-venous thrombosis were the most frequent arterial and venous TEs both at PV diagnosis and throughout the disease course, with a relative incidence of 50% and 32% respectively. The table compares the characteristics of patients who did or did not develop a TE after PV diagnosis. At univariate analysis, PV high risk status, a previous TE and hyperlipidemia at PV diagnosis were significantly associated with a subsequent TE. Among hematologic variables an elevated WBC count at the time of thrombosis, but not Hct or PLT levels, was highly significantly associated with the development of a TE. At multivariate analysis, WBC count ≥10.4 x 10^9/L and hyperlipidemia maintained their independent prognostic value, while high risk status and a previous TE lost their prognostic significance. Both at univariate and multivariate analysis, hyperlipidemia at diagnosis (P=0.009 and P=0.002) and high WBC count at thrombosis (P=0.001 and P=<0.0001) predicted for arterial thromboses, while only a history of prior thrombosis (P=0.03) predicted for venous ones.
In conclusion, our analysis confirms that elevated WBC count at the moment of the event more than increased hematocrit is associated to the development of thrombosis in PV pts. We also found that hyperlipidemia was an independent risk factor for arterial thrombosis, calling for an accurate management of increased lipid levels. Whether a reduction of the WBC count during the course of PV may reduce the frequency of TE remains to be demonstrated by prospective studies.
D'Adda:Novartis: Other: Advisory board; Incyte: Other: Advisory board; Pfizer: Other: Advisory board. Rossi:Daiichi Sankyo: Consultancy, Honoraria; Sanofi: Honoraria; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees; Novartis: Other: Advisory board; Alexion: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria; Celgene: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; Jazz: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal